It can be tricky to know when your child needs medical care, including who to contact and when. It is important you trust your instincts and get the help your child needs. Not getting the advice and treatment at the right time could put your child at risk of serious illness.
If your child already has a health condition (like asthma, diabetes, epilepsy) look out for warning signs that their condition is less well controlled. Follow the advice given to you by the medical team that look after your child.
Below is some information on different conditions. One symptom on its own may not always be serious. Use this information as an idea on what symptoms to look out for and who to contact.
Some symptoms might be a sign that your child could be seriously ill and your child needs to go to the hospital’s emergency department (A&E).
One symptom within a group below: talk to a health professional for advice today.
More than one symptom within a group below: contact your GP or 111 straight away.
Headache and/or Stiff Neck

One symptom below: talk to a health professional for advice today.
More than one symptom below: contact your GP or 111 straight away.
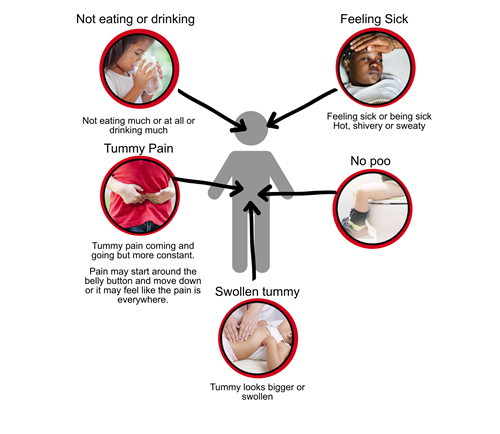
One symptom below: talk to a health professional for advice today.
More than one symptom below: contact your GP or 111 straight away.
In boys if they have lower tummy pain, are feeling sick or being sick and maybe a fever (high temperature and feel hot) check if the pain is coming from the scrotum (balls).
This is not common but it can happen after exercise or an injury to the groin. The symptoms often start in the night or first thing in the morning.
Sickness and Runny Poos
 One symptom below: talk to a health professional for advice today.
One symptom below: talk to a health professional for advice today.
More than one symptom below: contact your GP or 111 straight away.
If you also notice swelling - including on the legs, feet and ankles or any unexplained bruises please contact your GP or 111 straight away.
Fever
 If your baby has a fever and is less than three months old, even if they have no other symptoms, contact your GP or 111 straight away.
If your baby has a fever and is less than three months old, even if they have no other symptoms, contact your GP or 111 straight away.
A fever and one symptom below: talk to a health professional for advice today.
A fever and more than one symptom below: contact your GP or 111 straight away.
Always let the Doctor know if your child has not had any vaccinations / is not immunised and they have any of these symptoms.
Wheeze or Persistent Cough
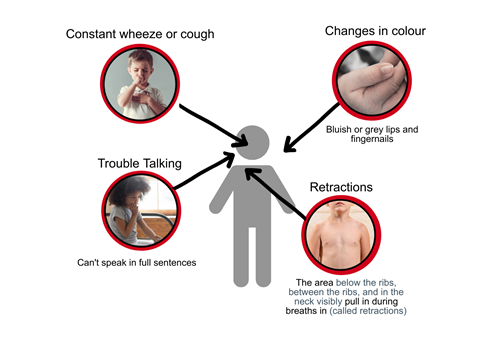 One symptom below: talk to a health professional for advice today.
One symptom below: talk to a health professional for advice today.
More than one symptom below: contact your GP or 111 straight away.
Very Thirsty & Tired
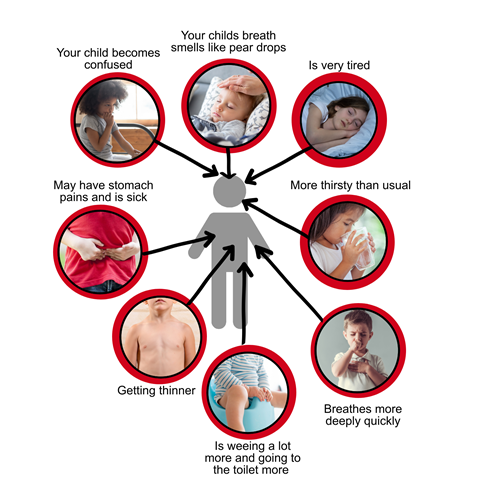 Contact you GP straight away or 111 out of hours if your child becomes;
Contact you GP straight away or 111 out of hours if your child becomes;
Call 999/ go to hospital emergency department (A&E) straight away if as well as the above;
Hepatitis
Since January 2022 there has been an small increase in the number of children with hepatitis in the UK. Hepatitis can cause the liver to become swollen and can be caused by infection with a virus. This is still very rare in the UK but trust your instincts if you are worried and call your GP.
Hepatitis symptoms include:
• Yellowing of the white part of the eyes or skin
• Dark wee
• Pale, grey-coloured poo
• Itchy skin
• Muscle and joint pain
• A high temperature
• Feeling and being sick
• Feeling unusually tired all the time ( sleeping more or seems drowsy)
• Loss of appetite
• Tummy pain.
If your child develops symptoms that could be due to a virus, such as a cold, vomiting or diarrhoea, the chance of them developing hepatitis is extremely low. Most children will soon recover if they have rest and drink plenty of water.
You do not need to contact the NHS unless your child is very unwell. For example, has breathing difficulties or is not eating or drinking, or if they develop jaundice (yellowing of the eyes or skin).
If your child is getting rapidly worse or you are worried, trust your instincts and contact your GP or call the NHS on 111.
NHS services are available to take care of you and make sure you get the advice and care you need.
If you are not sure whether your child is seriously unwell, call 111 or your GP for advice. Remember that you know your child best. If you think your child is seriously unwell, call 999 for an ambulance or go to your nearest A&E department.
You can contact the Healthy Child Service team by calling Just One Number on 0300 300 0123 or texting Parentline on 07520 631 590. Our opening hours are Monday to Friday, 9am to 5pm (excluding bank holidays).
If your child is 11-24 years old, FYI Norfolk is an interactive NHS website just for them. It provides reliable and trustworthy advice and support on lots of health and wellbeing topics.
 The Lullaby Trust - Baby Check App- This app has simple checks that you can do if your baby is ill and helps you think about whether they need to see a doctor or health professional.
The Lullaby Trust - Baby Check App- This app has simple checks that you can do if your baby is ill and helps you think about whether they need to see a doctor or health professional.